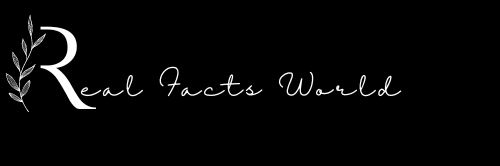
Saddle Pulmonary Embolism
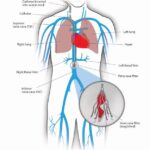
Saddle pulmonary embolism is a type of pulmonary embolism (PE) that occurs when a blood clot, usually from the legs or pelvis, travels through the bloodstream and lodges in the pulmonary artery, which is the main blood vessel supplying the lungs. A saddle pulmonary embolism is called such because the clot lodges at the point where the pulmonary artery branches out like a saddle.
This type of PE is considered more severe than other types of PE because it can block blood flow to both lungs, causing significant damage to lung tissue and reducing the amount of oxygen that can be delivered to the body’s organs.
Saddle pulmonary embolism is a medical emergency and requires prompt diagnosis and treatment to prevent serious complications such as cardiac arrest or sudden death. Treatment may involve medications to dissolve the clot and prevent further clots from forming, or in some cases, surgical intervention may be necessary.
What are the symptoms of saddle PE?
The symptoms of saddle PE can vary from mild to severe and may include: (1)
- Sudden onset of chest pain
- Shortness of breath
- Rapid breathing
- Rapid heart rate
- Low blood pressure
- Dizziness
- Fainting
- Coughing up blood
- Sweating
Causes Of Saddle Pulmonary Embolism
The most common cause of saddle pulmonary embolism is a blood clot that forms in the veins of the legs or pelvis. This type of clot is called a deep vein thrombosis (DVT) and can occur due to several factors such as:(2)
- Prolonged immobilization: E.g. during long-distance travel
- Surgery: Major surgeries, especially those that involve the legs or pelvis.
- Cancer: Some types of cancer.
- Pregnancy and childbirth: Hormonal changes during pregnancy and childbirth.
- Obesity: Being overweight or obese.
- Inherited blood clotting disorders: Certain genetic conditions.
- Smoking: Smoking can damage the lining of blood vessels.
- Certain medications: Certain medications, such as hormone replacement therapy or birth control pills.
It’s important to note that not everyone who has one of these risk factors will develop a saddle pulmonary embolism, and sometimes a saddle PE can occur without any apparent risk factors.
Read More: 9 Cluster headache home remedy
Read More: Does Anemia Cause Weight Loss or Gain?
Diagnosing Saddle Pulmonary Embolism
Diagnosing a saddle pulmonary embolism (PE) can be challenging because its symptoms can be similar to those of other conditions, such as pneumonia or heart attack. However, there are several tests that can be done to help diagnose a saddle PE, including:(3)
- CT pulmonary angiography (CTPA):
This is the most common test used to diagnose a saddle pulmonary embolism. It involves injecting a contrast dye into a vein and then taking images of the lungs using a CT scanner. The dye helps highlight any blood clots in the pulmonary arteries.
- Ventilation-perfusion (V/Q) scan:
This test involves injecting a radioactive substance into a vein and then taking images of the lungs using a special camera. The images can show if there are any areas of the lungs that are not getting enough blood flow or if there are any blood clots present.
- Doppler ultrasound:
This test involves using sound waves to create images of the veins in the legs and pelvis. It can detect if there are any blood clots present.
- Blood tests:
Blood tests can be done to check for markers of clotting, such as D-dimer. If a saddle pulmonary embolism is suspected, immediate medical attention is required. Treatment should not be hampered for diagnostic testing.
If a saddle pulmonary embolism is confirmed, treatment will typically involve medications to dissolve the blood clot and prevent further clots. In some cases, surgical intervention may be necessary.(4)
Saddle Pulmonary Embolism Treatment
The treatment of saddle pulmonary embolism (PE) is aimed at preventing further blood clots from forming, reducing the size of the existing clot, and improving blood flow to the lungs. Treatment typically involves a combination of medication and, in some cases, surgery.(5)
Anticoagulant Medications
Anticoagulant medications are typically the first line of treatment for saddle pulmonary embolism. These medications work by thinning the blood and preventing new clots from forming. Common anticoagulants include Heparin and Warfarin. In some cases, newer anticoagulants such as Dabigatran, Rivaroxaban, and Apixaban may also be used.
-
Heparin
Heparin is typically given as an intravenous (IV) infusion in the hospital setting. The initial dose is usually 80 units/kg followed by a continuous infusion of 18 units/kg/hour.
The dose is adjusted based on frequent blood tests to monitor the clotting time (activated partial thromboplastin time or APTT). Heparin is typically continued for a few days until the patient can transition to oral anticoagulant therapy.
-
Warfarin
Warfarin is an oral anticoagulant that is typically started after a few days of heparin therapy. The dose of warfarin is adjusted based on blood tests that measure the clotting time (international normalized ratio or INR).
The goal INR for saddle PE is typically between 2.0 and 3.0. The initial dose of warfarin is usually 5-10 mg/day, and the dose is adjusted based on the INR results.
-
Dabigatran
Dabigatran is an oral anticoagulant that is typically started after a few days of heparin therapy. The usual dose is 150 mg taken twice daily. However, the dose may be adjusted based on the patient’s kidney function, age, and weight. Dabigatran does not require routine blood tests like warfarin.
-
Rivaroxaban
Rivaroxaban is an oral anticoagulant that is typically started after a few days of heparin therapy. The usual dose is 15 mg taken twice daily for the first three weeks, followed by 20 mg taken once daily. The dose may be adjusted based on the patient’s kidney function and weight.
-
Apixaban
Apixaban is an oral anticoagulant that is typically started after a few days of heparin therapy. The usual dose is 10 mg taken twice daily for the first seven days, followed by 5 mg taken twice daily. The dose may be adjusted based on the patient’s age, weight, and kidney function.
It’s important to note that the dosages of these medications can vary depending on the individual patient’s characteristics and medical history. The dosages should always be determined and monitored by a qualified healthcare provider.
Thrombolytic Therapy
Thrombolytic therapy involves the use of medications such as tissue plasminogen activator (tPA) to dissolve the blood clot. This treatment is typically reserved for severe cases of saddle pulmonary embolism where there is a high risk of complications.
Inferior Vena Cava (IVC) Filter
An IVC filter is a small device that is inserted into the inferior vena cava, the main vein that carries blood from the lower body to the heart.
The filter traps any blood clots before they can reach the lungs. This treatment is typically reserved for patients who cannot tolerate anticoagulant therapy.
Embolectomy
In some cases, surgery may be needed to remove the blood clot. This is known as an Embolectomy and involves removing the clot from the pulmonary arteries. This treatment is typically reserved for severe cases where other treatments have been unsuccessful.
It’s important to note that treatment for saddle pulmonary embolism should be started as soon as possible to prevent complications such as Pulmonary Infarction or Cardiac Arrest.Treatment should be individualized for each patient based on their specific condition and underlying health status.
Prognosis Of Saddle Pulmonary Embolism
The prognosis of saddle pulmonary embolism (PE) can vary depending on several factors such as the size and location of the clot, the presence of underlying medical conditions, and the timeliness and effectiveness of treatment.
Saddle pulmonary embolism is considered a severe form of Pulmonary Embolism, with a higher risk of mortality compared to other types of Pulmonary Embolism. According to a study published in the Journal of the American Medical Association, the 30-day mortality rate for patients with saddle PE was 25%, compared to 11% for patients with non-saddle PE.
The study also found that patients with saddle PE were more likely to experience cardiac arrest, shock, and respiratory failure. However, early recognition and treatment of saddle PE can improve outcomes. The use of anticoagulant medications, thrombolytic therapy, and surgical intervention can all be effective in treating saddle PE and reducing the risk of complications.
Read More- Rubella IgG Positive Is Good Or Bad
A study published in the Journal of Thrombosis and Haemostasis found that patients who received thrombolytic therapy had a lower mortality rate compared to those who received anticoagulant therapy alone. The study also found that patients who received thrombolytic therapy had a higher risk of bleeding complications.
It’s important to note that the prognosis of saddle PE is highly individualized and can vary depending on the specific patient’s medical history and response to treatment. Close monitoring and follow-up with a healthcare provider is essential for the optimal management of saddle pulmonary embolism.(6)(7)
Saddle Pulmonary Embolism Risk Factors
There are several risk factors that can increase the likelihood of developing saddle PE. Below are some of the most common risk factors, along with a reference study that provides additional information:
- Previous history of blood clots:
Individuals who have had a previous blood clot, such as deep vein thrombosis (DVT), are at increased risk for developing Saddle Pulmonary Embolism. According to a study published in the Journal of Thrombosis and Haemostasis, the risk of developing Pulmonary Embolism is highest in the first three months following a DVT diagnosis.
- Prolonged immobility:
Prolonged periods of sitting or standing can increase the risk of developing blood clots in the legs, which can then travel to the lungs and cause saddle pulmonary embolism. A study published in the Journal of Vascular Surgery found that prolonged air travel, such as flights lasting over 8 hours, was associated with an increased risk of developing Pulmonary Embolism.
- Surgery or trauma:
Major surgeries or traumatic injuries can increase the risk of developing blood clots and saddle pulmonary embolism. A study published in the Annals of Surgery found that patients who underwent major abdominal surgery had a higher risk of developing Pulmonary Embolism compared to patients who underwent minor surgery.
- Cancer:
Certain types of cancer, such as lung cancer and pancreatic cancer, can increase the risk of developing blood clots and saddle pulmonary embolism. A study published in the Journal of Thrombosis and Haemostasis found that cancer patients were more likely to develop PE compared to non-cancer patients.
- Obesity:
Obesity is a known risk factor for a variety of health conditions, including saddle PE. A study published in the Journal of Thrombosis and Haemostasis found that obese individuals had a higher risk of developing Pulmonary Embolism compared to non-obese individuals.It’s important to note that the presence of one or more of these risk factors does not necessarily mean that an individual will develop saddle PE.
However, individuals who are at increased risk should take steps to reduce their risk, such as maintaining a healthy weight, staying active, and avoiding prolonged periods of immobility. Additionally, healthcare providers may recommend preventative measures, such as anticoagulant therapy, for individuals who are at high risk for Saddle Pulmonary Embolism. (8)
Preventing Saddle Pulmonary Embolism
Below are some strategies that can help prevent saddle PE:
- Maintain a healthy weight:
Obesity is a known risk factor for saddle PE. Maintaining a healthy weight through a balanced diet and regular exercise can help reduce the risk of developing saddle PE.
- Stay active:
Regular physical activity can help improve circulation and prevent blood clots. According to the American Heart Association (AHA), adults should aim for at least 150 minutes of moderate intensity exercises per week.
- Avoid prolonged periods of immobility:
Prolonged periods of sitting or standing can increase the risk of developing blood clots, which can then travel to the lungs and cause saddle PE. Individuals who must sit or stand for long periods of time, such as during air travel or desk work, should take frequent breaks to move around and stretch.
- Use compression stockings:
Compression stockings can help improve circulation in the legs and reduce the risk of blood clots. According to a study published in the Journal of the American Medical Association, the use of compression stockings during air travel can significantly reduce the risk of developing PE.
- Take anticoagulant medication:
For individuals who are at high risk for saddle PE, healthcare providers may recommend anticoagulant medication to help prevent blood clots from forming.
A study published in the New England Journal of Medicine found that the use of anticoagulant medication significantly reduced the risk of recurrent blood clots in individuals who had previously experienced a blood clot.
Read More: Vaginal Boils: How to Prevent Them and Keep Your Intimate Area Healthy
It’s important to note that the most effective strategy for preventing saddle PE will vary depending on an individual’s specific risk factors and medical history. Healthcare providers can help assess an individual’s risk and recommend preventative measures accordingly.(9)
Saddle Pulmonary Embolism Survival Rates
The survival rate for saddle PE can vary depending on the severity of the condition and how quickly it is diagnosed and treated.
According to a study published in the Journal of Thrombosis and Haemostasis, the mortality rate for saddle PE ranges from 10% to 65%, with higher rates observed in patients who are older or have comorbidities such as heart failure or cancer. The study also found that mortality rates were significantly lower in patients who received prompt treatment with anticoagulant medication and/or thrombolytic therapy.(10)
Conclusion:
In conclusion, saddle pulmonary embolism is a severe condition that can cause significant harm to the patient. It is essential to seek medical attention immediately if you experience any symptoms of SPE. With early diagnosis and treatment, most patients can recover fully from this condition. By taking steps to prevent blood clots from forming, you can reduce your risk of developing saddle pulmonary embolism and other related conditions.
9 thoughts on “Saddle Pulmonary Embolism: Symptoms You Should Not Ignore (2023)”